Autoimmune diseases develop when the immune system mistakenly attacks the body’s own tissues by recognizing self-antigens as threats. This often results in persistent inflammation and tissue injury. Among the numerous autoantibodies involved in these disorders, anti-double-stranded DNA (anti-dsDNA) antibodies are particularly significant for both diagnosis and management. They are crucial biomarkers, especially in systemic lupus erythematosus (SLE). By targeting the host’s DNA, these antibodies initiate a series of immune responses that drive disease progression.
Biology of anti-dsDNA antibodies
When B cells encounter extracellular DNA or nucleosomes released by dying cells, such as those undergoing apoptosis or necrosis, they can internalize and present these host molecules as antigens. With assistance from T helper cells, B cells differentiate into plasma cells that secrete anti-dsDNA antibodies. Over time, these antibodies can undergo class switching to high-affinity immunoglobulin G (IgG), increasing their pathogenic potential.
The production of anti-dsDNA antibodies occurs when central and peripheral tolerance mechanisms fail to eliminate autoreactive B cells. Several factors contribute to this breakdown in immune tolerance, including genetic predisposition and environmental triggers such as ultraviolet radiation, chemical exposures, infections, and hormonal influences.
Pathogenic Mechanisms
The presence of anti-dsDNA antibodies is closely associated with tissue damage in autoimmune diseases, particularly systemic lupus erythematosus (SLE). These antibodies drive disease progression through several interrelated pathogenic mechanisms.
A primary mechanism involves the formation of immune complexes, where anti-dsDNA antibodies bind to circulating host DNA. These immune complexes deposit in target tissues—such as the kidneys, skin, joints, and blood vessels—triggering local inflammation and complement activation. The ensuing complement cascade recruits inflammatory mediators, leading to chronic inflammation, tissue injury, and organ dysfunction.
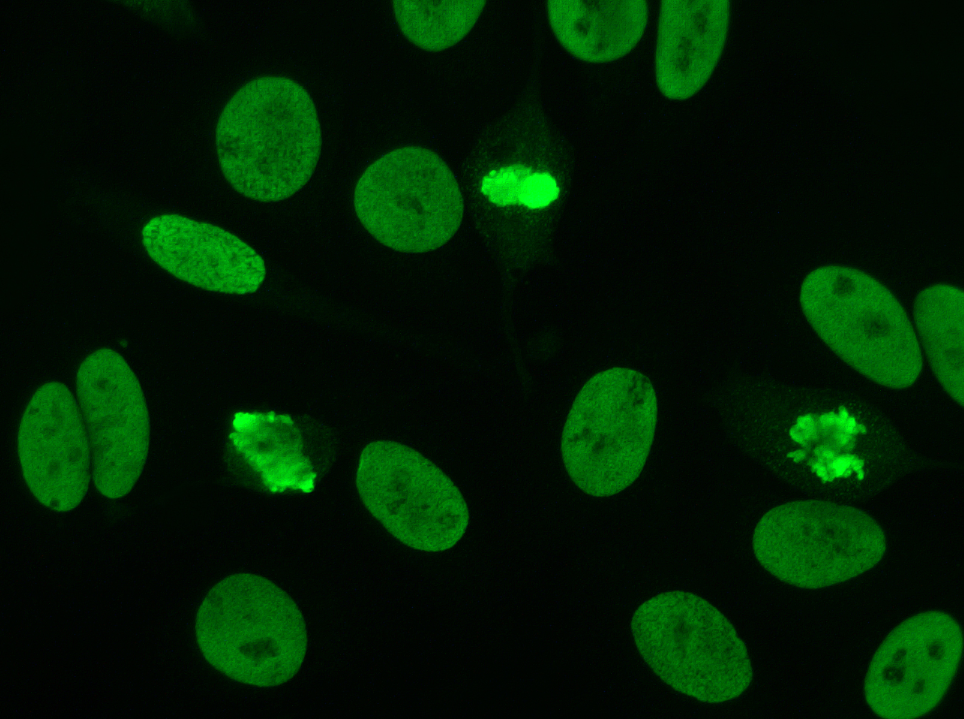
Beyond immune complex formation, anti-dsDNA antibodies can directly penetrate living cells and bind to nuclear DNA, inducing cytotoxic effects and promoting cell death by apoptosis or necrosis. The release of intracellular material from dying cells perpetuates a cycle of continuous immune activation.
Cross-reactivity further amplifies tissue damage. Anti-dsDNA antibodies may mistakenly target other cellular or extracellular components, such as α-actinin, a cytoskeletal protein, thereby exacerbating inflammation, particularly in organs like the kidneys during lupus nephritis.
Additionally, anti-dsDNA antibodies can activate intracellular toll-like receptors (TLRs), including TLR-7 and TLR-9, within dendritic cells. This activation stimulates the production of type I interferons, potent cytokines that enhance the survival and activation of autoreactive B and T cells, further aggravating autoimmunity and sustaining chronic tissue damage.
Together, these diverse pathogenic actions highlight the central role of anti-dsDNA antibodies in the development and progression of autoimmune disease.
Anti-dsDNA in SLE
- Diagnostic specificity: Anti-dsDNA antibodies exhibit up to 98% specificity for SLE. However, not all SLE patients produce these antibodies limiting its use for detection of the disease.
- Disease activity marker: Anti-dsDNA titers correlate with disease activity. For example, rising levels of these antibodies may be observed before disease flares, while declining levels indicate remission.
- Prognostic relevance: High and persistent anti-dsDNA titers often predict severe organ involvement, particularly renal complications.
Detection methods
Different techniques are used in laboratories to detect and measure anti-dsDNA antibodies. Each assay differs in sensitivity, specificity, and utility.
- Farr assay (Radioimmunoassay): It detects high-avidity antibodies with high specificity and sensitivity. Clinicians use it to confirm SLE and monitor lupus nephritis. The requirement for radioactive materials limits its practical use.
- ELISA (Enzyme-linked immunosorbent assay): It offers high sensitivity and detects both high- and low-affinity antibodies. However, it may give false positives.
- Crithidia luciliae immunofluorescence test (CLIFT): This test uses the kinetoplast of Crithidia luciliae as a source of pure dsDNA. It detects high-avidity antibodies and provides high specificity.
- Chemiluminescence and multiplex immunoassays: This provides automated, high-throughput detection. It is being increasingly used for routine monitoring.
Clinical correlation
Elevated anti-dsDNA antibody titers are associated with lupus nephritis, whereas fluctuating levels indicate changes in disease activity. They are also implicated in neurological manifestations of lupus, including autoimmune cerebritis.
Presence in other autoimmune diseases
Although highly specific for SLE, low titers of anti-dsDNA antibodies occasionally appear in other conditions such as rheumatoid arthritis, autoimmune hepatitis, Sjögren’s syndrome, and mixed connective tissue disease. However, their presence in these disorders is less specific and often lacks the strong clinical correlation seen in SLE, particularly with renal involvement. Therefore, their diagnostic significance remains most pronounced in SLE.
Therapeutic implications
Targeting anti-dsDNA antibodies has emerged as a potential therapeutic strategy. Anti-dsDNA antibody titers provide useful information in guiding and evaluating treatment.
- Monitoring therapy: Decreasing levels of anti-dsDNA antibodies reflect effective immunosuppression and disease control.
- Targeted treatments: Biologic agents such as rituximab and belimumab target B-cell pathways involved in antibody production.
- Experimental approaches: Some therapies under investigation include inhibitors of plasma cells and antigen presentation pathways.
Emerging research directions
Recent advances aim to refine the utility and understanding of anti-dsDNA antibodies beyond their established diagnostic value in systemic lupus erythematosus. Studies are increasingly focusing on their pathogenic mechanisms, including how they interact with nucleosomes and cross-react with renal and vascular antigens, contributing to tissue damage.
Researchers are also exploring their involvement in non-SLE autoimmune conditions and their potential as biomarkers for disease activity, prognosis, and treatment response. Advances in epitope mapping, affinity profiling, and novel detection techniques are enhancing our understanding of anti-dsDNA antibodies’ specificity and functional diversity, paving the way for more targeted therapeutic approaches.
Conclusion
Anti-dsDNA antibodies play a crucial role in the diagnosis, monitoring, and pathogenesis of autoimmune diseases, especially systemic lupus erythematosus (SLE). Their levels often correlate with disease activity, reinforcing their value as reliable biomarkers. While they can occasionally appear in other autoimmune conditions, their diagnostic relevance is most pronounced in SLE. Ongoing research continues to reveal broader functions and highlights their potential as therapeutic targets. Improvements in detection techniques and deeper insights into their pathogenic mechanisms may pave the way for more precise and personalized strategies in autoimmune disease management.